Breaking barriers
February 27, 2020 @ 8:00am
An easier and more accurate method to test for cervical cancer is paving the way for women’s health writes Syida Lizta Amirul Ihsan
MALAYSIA is on its way to eliminating cervical cancer with the adoption of human papillomavirus (HPV) testing. It will significantly increase the screening rate as the method is easier (via self-sampling) and more accurate.
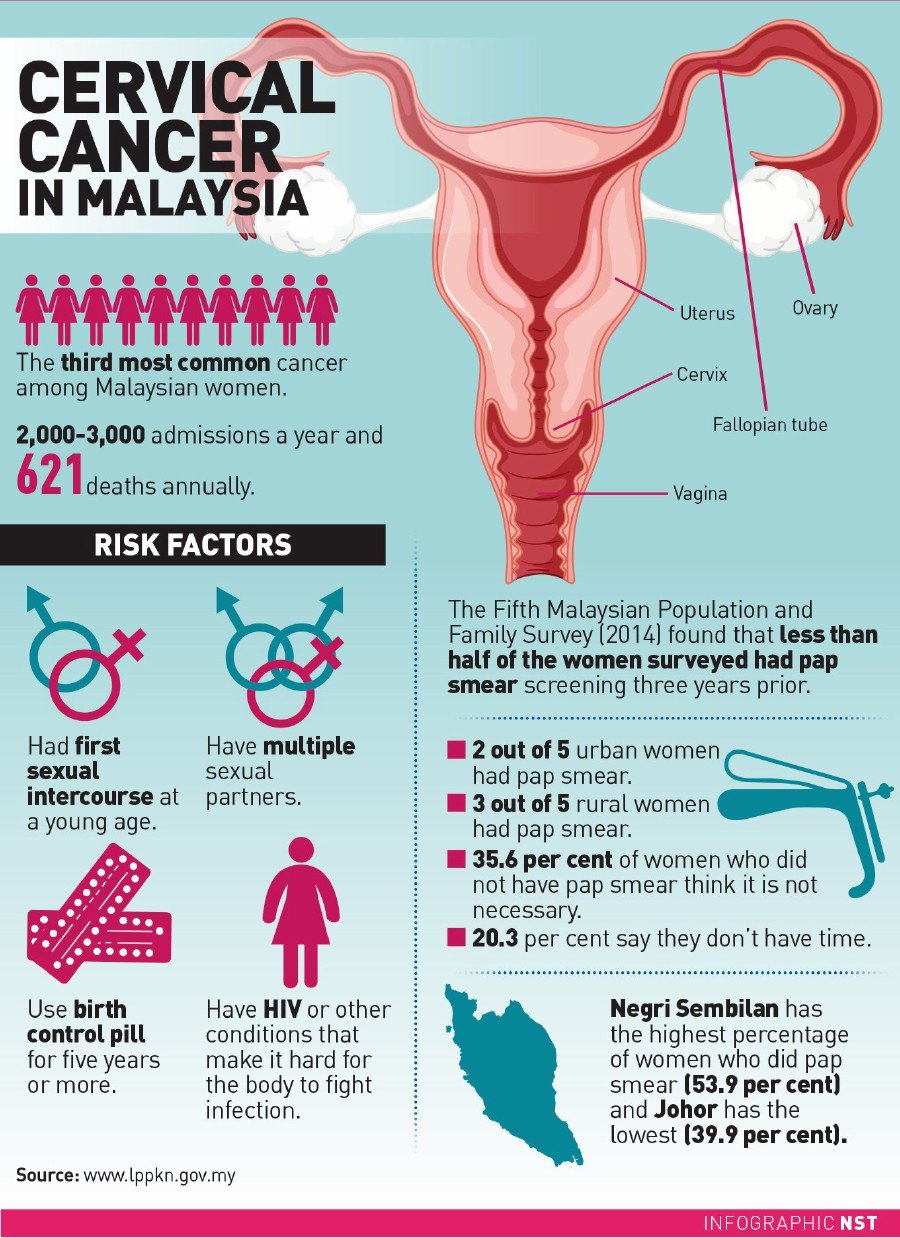
Traditionally, cervical cancer— the third most common cancer among Malaysian women — is diagnosed through a pap smear, where a speculum is inserted into the vagina.
The doctor then uses a swab to collect a sample to detect any cellular changes on the wall of the cervix.
A pap smear costs between RM40 and RM80 but many women shy away from it because they find it embarrassing and inconvenient.
Last week, Universiti Malaya Medical Centre and VCS Foundation of Australia launched the Rose Foundation and Laboratory, an extension of the Rose Programme which started last year and which kicked off its nationwide screening campaign in July.
It was officiated by Energy, Science, Technology, Environment and Climate Change deputy minister Isnaraissah Munirah Majilis.
Rose Foundation medical technical advisor Prof Dr Woo Yin Ling says currently, only 12 per cent of women go for pap smears, leaving a big group vulnerable to the disease.
“This programme eliminates the social and health barriers to having these women screened. The adoption of mobile technology and molecular testing is transforming the field.”

DO IT YOURSELF
The Rose solution, says Dr Woo, integrates three components.
The first is a convenient self-sampling method using a swab which a patient does herself. She then returns the sample and the Rose Laboratory at Universiti Malaya will process it. The result will be sent via SMS on her mobile phone within three weeks.
The second component is the HPV testing.
“Instead of detecting cellular changes, this test looks for HPV DNA before the changes take place, so irregularities are caught earlier.”
Unlike a pap smear which should be done every three years, a negative result on a HPV test requires the patient to be tested again only after five to 10 years.
“The third is a digital platform where results are sent to mobile phones. This feature also ensures that results are linked to a government hospital for follow-up so these women need not worry about “getting lost in the system”.

Dr Woo says the aim of the Rose Foundation — similar to the Rose programme — is to get more women in the B40 group to go for screening. It’s offered at government clinics in Taman Medan, Port Klang and Kalumpang, Selangor.
“We have also engaged doctors, nurses and community volunteers and screened some 8,000 women in Perak, Johor, Sarawak, Sabah and Penang. Out of that, seven per cent tested positive and received follow-up,” she says.
“As the samples can be stored for up to 12 days, we are able to test women in very rural areas who otherwise do not have access to a hospital, much less a pap smear,” she says.
Women who are not in the B40 group but who wish to do the HPV test can take part in the Buy a Rose programme, in which the kit is sold for RM250.
Due to its ease and accuracy, the HPV test will one day phase out pap smears in detecting cervical cancer.
Dr Woo says adopting a new method requires trust, especially since this involves mobile technology.
“It’s pretty much like moving from cash to an e-wallet system. It takes time but with proper infrastructure and education, we will get there.”
For more information go to programrose.org, call 03-84082211 or email programrose@gmail.com